ABC News
by STEFAN P. KRUSZEWSKI, M.D.
"clients are continuing to rely heavily on pills to combat their anxieties, mood changes and addiction. "
In my specialty as an addiction psychiatrist, I have often advocated for residential treatment when unremitting drug and alcohol problems persist because other, less intensive, services have failed. That may soon change.
Over the past two years, I’ve witnessed a worrisome trend: the medicalization of addictions. Some of this makes no sense to me. Let me explain.
There have always been drug treatments for acute detoxification of drug and alcohol problems. The drugs have changed over the years, but the concept of providing a brief period of drug stabilization to prevent seizures or delirium or to mitigate psychosis has gone one unabated.
For instance, barbiturates were once used to minimize alcoholic delirium, but the barbiturates were replaced by benzodiazepines and, although still commonly in use, the benzodiazepines have been more recently supplanted or co-administered with anti-seizure drugs, like valproex or gabapentin. The endpoint has largely been the same: we will stabilize the patient over an acute period of rapidly changing health conditions (sweating, diarrhea, pulse, blood pressure, temperature, pain) and, once the detoxification has been successfully completed and the patient is comfortable and alert, we will begin a process of education and behavioral health techniques to foster a hoped-for drug free recovery state.
That is changing, however, in certain facilities in ways that I believe are destructive and counter-productive.
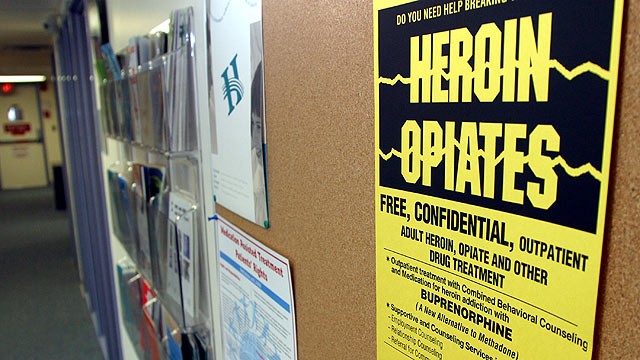
Two cases serve as illustration: I’m asked to review the medical necessity and reimbursement for care provided in a high profile and nationally-acclaimed drug rehab. The case is of a 20-year-old male from the northeastern United States who is addicted to a drug, methadone (an opioid agonist replacement medicine) and alprazolam, a benzodiazepine anti-anxiety drug. He enters treatment and spends 29 days in rehab, where he is provided buprenorphine (a partial opioid agonist replacement drug for opioid dependence) in decremented detox and maintenance for the duration of his stay and clonazepam (used as a substitute for his alprazelom addiction). He is discharged with the recommendation and prescription to return home and continue methadone and clonazepam.
That’s worth repeating. The patient is discharged to continue the same addictive drug for which he was admitted and a longer-acting (and still habit-forming) benzodiazepine drug to replace his other anti-anxiety medication. And with a price-tag of nearly $40,000.
Separately, I’m asked to review, for medically necessity and reimbursement purposes, the care of a 53-year-old woman. Like the young man in the above synopsis, she enters a world-class drug rehab in Florida, but this time for alcoholism. At the time of admission, she is also taking an SSRI antidepressant and a benzodiazepine anti-anxiety drug.
She spends 27 days in the facility. At various times during her admission, not unlike many individuals being weaned off alcohol, she complains of mood fluctuations, anxiety, sleeplessness and body aches. At the time of discharge, she has been taking — and she is recommended to continue to take — seven drugs: citalopram, an SSRI antidepressant; bupropion, an SNRI antidepressant; a small dose of an antipsychotic, aripiprazole, to augment the antidepressant effects of her two different antidepressants; a small dose of thyroid supplement, thyroxine, to do the same; gabapentin, an antiseizure medicine and clonazepam, both prescribed to decrease her anxiety; and carisoprodol, a centrally-acting anti-muscle spasm drug to minimize her musculoskeletal discomfort.
Capsulizing the above: A woman with alcohol dependence on one drug for depression is treated in rehab for almost a month (at a cost of a little more than $45,000) and is discharged on seven drugs, including not one, but two (clonazepam and carisoprodol) with significant habit-forming and addiction-enhancing characteristics.
Message to substance providers: We have a problem. Although addiction experts may justify these “treatments” because education and solace is provided to the patients, I believe that this mocks the purpose of (the very important and necessary) addiction treatment. There is little, if any, harm reduction, because the clients are prescribed the same or other addictive compounds during and after rehab. The clients are also prescribed new drugs, particular in the latter case of the alcoholic woman, whose potential for drug-drug interactions and future adverse events cannot be accurately predicted.
The clients are receiving expensive inpatient care for services and treatment that could easily be managed in cheaper and less-acute-care outpatient settings, like intensive outpatient or partial hospital programs. And, most importantly, the clients are continuing to rely heavily on pills to combat their anxieties, mood changes and addiction.
Problem? Relying on pills got them to rehab in the first place. So what’s the point of attending and paying for — or charging a commercial insurance carrier, Medicare or Medicaid, or any other third-party payer — for an expensive retreat that leaves you in virtually the same mental place, or worse, than you started? Not that much.
Dr. Stefan Kruszewski is an addiction psychiatrist and CEO of Kruszewski & Associates, a Harrisburg, Pa., company that focuses on health care and financial fraud.


SHARE YOUR STORY/COMMENT