The manual that psychiatrists use to diagnose mental disorders is too quick to classify moral lapses as full-blown pathologies.
The Los Angeles Times –
November 5, 2013
By Theodore Dalrymple
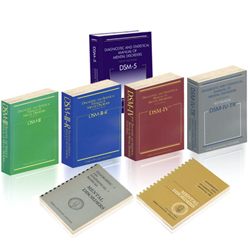
When the 1980 edition of the Diagnostic and Statistical Manual of Mental Disorders (commonly known as the DSM-3) was being prepared, psychiatrist Allen Frances lobbied for the inclusion of a new diagnosis: masochistic personality disorder. His push failed, and by the time the fourth edition came out in 1994 (edited by Frances), he was glad it had. He no longer believed such a condition existed.
Masochistic personality disorder, as Frances had conceived it, “diagnosed” those whose typical behavior brought them unhappiness by “self-sacrifice in the service of maintaining relationships or self-esteem.” The diagnosis might help explain women who put up with violently abusive lovers or husbands or repeatedly choose such men as sexual partners. Feminists attacked the proposed diagnosis, arguing that it blamed women for their own abuse. And it was on those grounds, not scientific ones, that the DSM-3 excluded the diagnosis.
In fact, the pattern of behavior that Frances’ disorder sought to categorize is common; I encountered it often in my clinical practice. “His eyes suddenly go funny,” a patient would say of a violent boyfriend, “like he’s having a fit. He stares, he doesn’t blink, and then he starts to strangle me. I don’t think he knows what he’s doing.”
“Would he do it in front of me, then?” I would ask, and the scales would fall, at least temporarily, from her eyes. But the willingness to excuse abusive behavior was often astonishing. I recall one patient with an arm and a jaw broken by a man just out of prison after a long sentence for killing another woman. She rejected our warning that she was in imminent danger and walked out of the hospital arm in arm with her abuser.
Frances was right, though, to later reject his diagnosis classification — not because masochistic behavior is a fiction but because a description of behavior is not the same as a medical diagnosis. We all show patterns of behavior, and some prove far from conducive to our own success or happiness. Such behavior does not make us ill, however, but weak and fallible.
No edition of the DSM, including the latest, recognizes a masochistic personality disorder. Yet the new DSM-5 does agree with abused women that their male abusers are suffering from a psychiatric condition: intermittent explosive disorder. The diagnostic criteria include having had three violent and unpremeditated outbursts in a 12-month period in which people or animals were hurt.
Leaving aside the question of why the diagnosis should require three rather than two or four behavioral outbursts in 12 months (or, for that matter, in six or 18 months), a question must be asked: Is the habit of losing one’s temper and destroying things or hurting people really a medical condition? Doesn’t the diagnosis empty the act both of meaning and moral content, all in the service of a spurious objectivity?
The notion of an outburst of temper grossly out of proportion to whatever provoked it — a factor necessary to the diagnosis — implies moral judgment as to what constitutes appropriate and inappropriate displays of anger. Appropriateness is an irreducibly moral concept, requiring conscious judgment; no number of functional MRI scans of the amygdala or of any other part of the brain will assist in that judgment.
To qualify as intermittent explosive disorder, the DSM-5 asserts, an individual’s outbursts should not have tangible ends, among them power and intimidation. Yet if we exclude such ends, it becomes inexplicable as to why outbursts should commonly occur in response to a minor provocation by a close intimate or an associate. To be devoid of tangible ends, the outbursts would have to occur completely at random, and they seldom do. The editors seem to have reflected little on the meaning of their own work.
 It is easy, of course, to lampoon psychiatric nosology — the system for classifying disorders — and to underestimate the difficulty of producing such classification. After all, no objective laboratory markers or correlatives of psychiatric disorder exist. Psychiatrists must show discretion in what they regard as genuine illness, and they will often be wrong. But no one who has encountered, say, a manic in full flight is likely to doubt that he is in the presence of illness.
It is easy, of course, to lampoon psychiatric nosology — the system for classifying disorders — and to underestimate the difficulty of producing such classification. After all, no objective laboratory markers or correlatives of psychiatric disorder exist. Psychiatrists must show discretion in what they regard as genuine illness, and they will often be wrong. But no one who has encountered, say, a manic in full flight is likely to doubt that he is in the presence of illness.
On the other hand, let’s consider “factitious disorder.” According to DSM-5, the illness consists of “falsification of physical or psychological signs and symptoms, or induction of injury or disease, associated with identified deception.” Should that really be considered in quite the same light as psychosis or mania? That is, should we grant the same status to someone pretending to be ill as to someone genuinely ill?
Yet this is precisely what the DSM-5 does, establishing its authors’ lack of common sense, the quality that psychiatrists, perhaps more than any other kind of doctor, need. The manual’s lack of common sense would be amusing were it not destined to be taken with superstitious seriousness by psychiatrists around the world, as well as by insurers and lawyers.
If the DSM-5 reflects the American Psychiatric Assn.’s views, then that organization clearly views humanity with Swiftian distaste. And that distaste is motivated, one suspects, by the hope of an endless supply of patients. For it stands to reason that a man in possession of a psychiatric disorder must be in want of a psychiatrist.
Theodore Dalrymple, a retired British doctor, is a contributing editor of City Journal and a Manhattan Institute fellow. This piece is adapted from the fall issue of City Journal.


SHARE YOUR STORY/COMMENT